The primary goal of the Kentucky Sexually Transmitted Disease Prevention and Control Program is to prevent the spread and complications of sexually transmitted diseases (STDs).
HEALTH ALERT
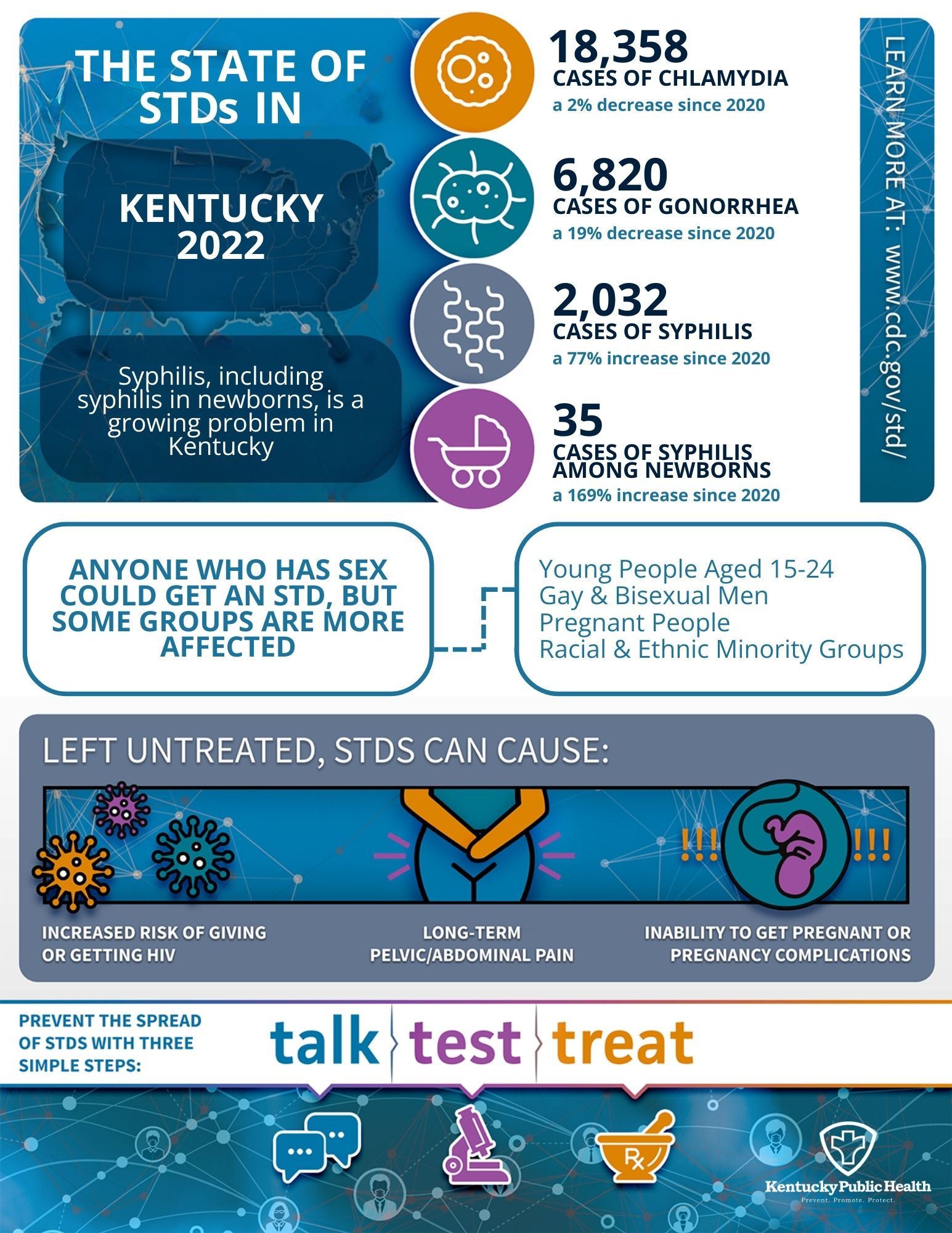
Syphilis is on the rise! The number of reported cases of congenital syphilis in Kentucky has risen from 2 cases in 2012 to 35 cases in 2022.
CDC | Syphilis
Diseases and Conditions:
Where to get help
Local Health Departments offer testing for Chlamydia, Gonorrhea, and Syphilis, and provide treatment for individuals diagnosed with, exposed to, or suspected of having these diseases. Patients with other sexually transmitted infections will receive counseling about the infection and will be referred to a healthcare provider, who can test for and treat these diseases.
Services received at local health departments are confidential. A service fee may be charged; however, patients will not be denied testing or treatment if they are unable to pay.
Data and Statistics
For information and statistical data requests, please contact the Kentucky STD Prevention and Control Program at (502) 564-4804.
Information for Healthcare Providers
STD Treatment Guidelines Recommended by CDC
2021 STD Treatment Guidelines
How to Report
Please report by phone or send confidential reports for STD cases on the EPID200 form by fax or mail to the Kentucky STD Prevention and Control Program state office or the local health department where the case resides.
Secured fax (502) 564-5715
Phone (502) 564-4804
Mail to
Kentucky Department for Public Health
STD Prevention and Control Program
275 East Main Street, MS HS2CC
Frankfort, KY 40621
Local Health Departments