Syringe Services Programs (SSP), also known as Syringe Exchange Programs (SEP), have existed and been studied extensively in the United States since 1988. Community-based SSPs provide access to sterile needles and syringes free of cost, facilitate safe disposal of used needles and syringes and offer safer injection education. SSPs in Kentucky also provide participants with access to critical services and programs, including substance use disorder treatment programs; overdose prevention education; screening, care and treatment for HIV and viral hepatitis; prevention of mother-to-child transmission; hepatitis A and hepatitis B vaccination; screening for other sexually transmitted diseases and tuberculosis; partner services; and other medical, social and mental health services.
Prior to 2015, certain harm reduction strategies, such as Syringe Services Programs, were prohibited by law. However, in 2015, a significant change in legislation shifted how harm reduction strategies were allowed to be implemented in Kentucky. Senate Bill 192 granted approval for Local Health Departments to operate substance abuse treatment outreach programs which allowed the exchange of hypodermic syringes. The law states that items exchanged at the programs shall not be deemed drug paraphernalia while located at the program.
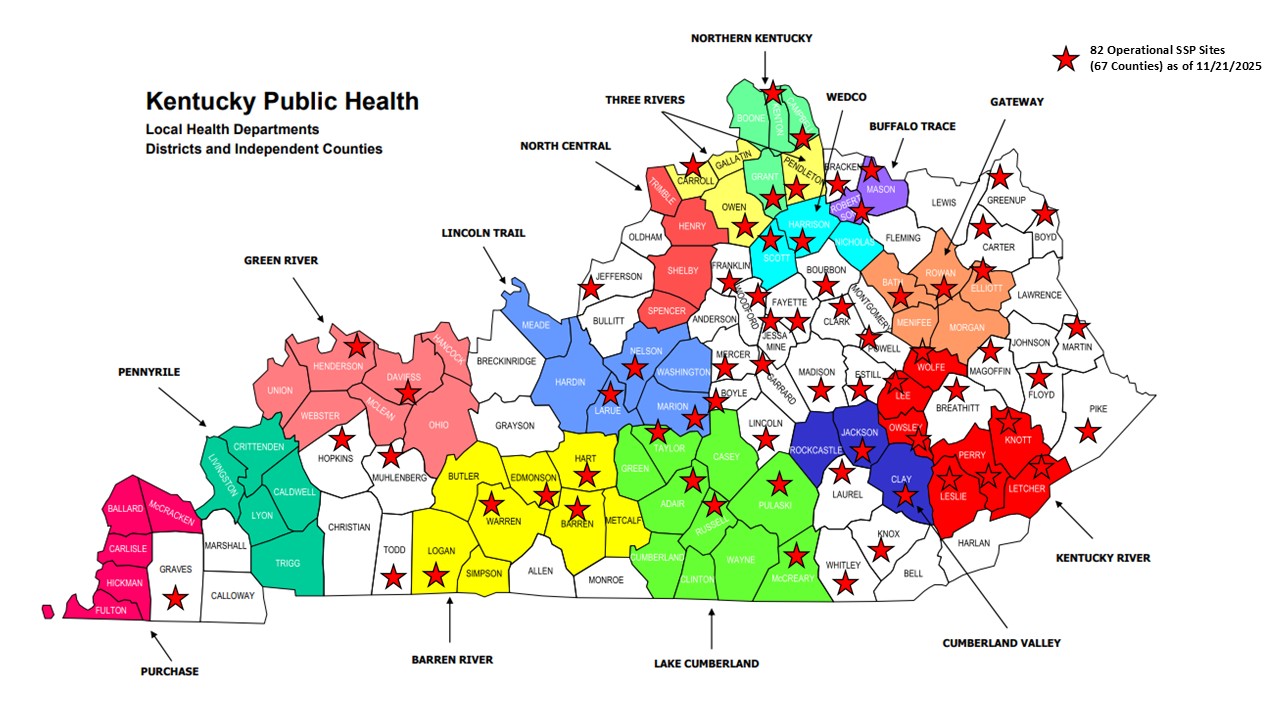
Very soon after the change in legislation, the Kentucky Department for Public Health published guidelines for Local Health Departments implementing SSPs. Since that time, more 80 SSP sites are operating in 66 counties throughout Kentucky.
Senate Bill 192 impacts KRS 218A.500
KY SSP Guidelines (Long Version)
KY SSP Guidelines (Short Version)
*Please contact
Chase Barnes to revise SSP locations and hours.
Facts about SSPs
- SSPs do not encourage the initiation of drug use nor do they increase the frequency of drug use among current users. (1)
- SSPs reduce the spread of infections like HIV and viral hepatitis. (2)
- SSPs do not increase community crime. Community residents may worry that syringe services locations will increase theft, sex trades, assaults, and an increase of contaminated needles on the street. However, studies have shown that SSPs actually decrease crime in the area they are located. (3)
- SSPs increase community safety. Research shows that SSPs promote public health and safety by taking syringes off the streets and protecting law enforcement personnel from needle stick injuries, which can result in the transmission of diseases such as HIV/AIDS and hepatitis B and C. (4)
- SSPs connect people to treatment. One study found that SSP participants are five times more likely to enter a drug treatment program than nonparticipants. (5)
Recommended Best Practices for Effective SSPs in the United States
SSPs are central to reducing disease and other health burdens among people who inject illicit drugs. Three decades of research has demonstrated the effectiveness of SSPs in preventing HIV and other blood-borne infections, as well as connecting people who inject drugs with a range of vital medical and social services and supports.
The Recommended Best Practices report from the New York City Department of Health and Mental Hygiene with the Drug Policy Alliance summarizes the consensus among United States SSP experts of the underlying principles and programmatic elements that enable or constrain SSP effectiveness. Effective SSPs have the support of local governing bodies and match sound operational characteristics with responsiveness to the unique features of their host communities. New or expanding SSPs may benefit from technical assistance from the considerable expertise of those experienced in operating SSPs around the country. The panel highlighted operational characteristics that are critical for effective SSPs, and measures to be avoided because they undermine the primary goal of SSPs: to make new, sterile syringes available to Persons Who Inject Drugs (PWIDs).
Characteristics of Effective SSPs (6)
- Promote secondary syringe distribution
- Train and support peer educators
- Do not impose limits on number of syringes (doing so promotes sharing of needles)
- Maximize responsiveness to characteristics of the local PWID population
- Adapt planning activities and service modalities to subgroup needs
- Provide or coordinate the provision of other health and social services
- Used Syringes are Dangerous
- How to Clean Your Syringes
- Include diverse community stakeholders in creating a social and legal environment supportive of SSPs
SSP Practices to Avoid (6)
- Supplying single-use syringes
- Limiting frequency of visits and number of syringes
- Requiring one-for-one exchange (results in sharing of needles)
- Imposing geographic limits
- Restricting syringe volume with unnecessary maximums
- Requiring identifying documents
- Requiring unnecessary data collection
Naloxone Availability and Overdose Response Education
What is naloxone?
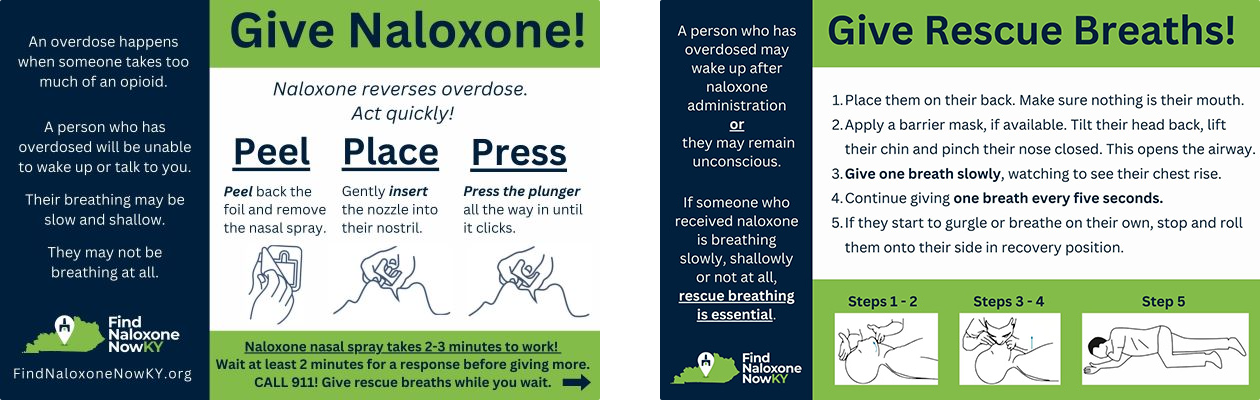
Naloxone is a medication that temporarily reverses opioid overdose. It works by blocking the effects of opioids on the brain. To find out where you can receive naloxone at no-cost, visit www.FindNaloxoneNowKY.org.
An opioid overdose happens when someone takes too much of an opioid. They become unconscious and their breathing begins to shut down. If an overdose is not reversed, it's likely that this person will stop breathing and die. That's why it's important to give naloxone quickly when you suspect an opioid overdose.
How is naloxone administered?
Knowing how to administer naloxone properly is just as important as recognizing the signs and symptoms of an opioid overdose. Because individuals have different learning styles, www.FindNaloxoneNowKY.org offers access to the trainings in a variety of formats:
- a thorough, five-step training that can be printed on a business card,

How is naloxone distributed throughout Kentucky?
Strategic planning for naloxone distribution focuses on getting naloxone to people likely to witness overdose in the communities where it's needed most. See Kentucky's 2025-2026 Naloxone Saturation Plan to learn more about this approach.
Single Signature Naloxone Prescription: Purpose
Pharmacists are uniquely positioned to help reduce morbidity and mortality associated with opioid overdose by dispensing naloxone to at-risk patients or their friends and family members, and educating them on the proper use of these products. This non-patient specific prescription (standing order) authorized by the Kentucky Department for Public Health (KDPH) establishes the protocol that allows Kentucky-licensed naloxone protocol trained pharmacists to dispense naloxone to at-risk patients and third parties in pharmacies located in Kentucky.
Print the form below to be registered in the KDPH program. This non patient-specific prescription is valid for one year from the date authorized.
Download and Print the Single Signature Prescription Form